New GLP-1 Nutrition Insights: How will this change your practice?
Key insights from the new joint advisory statement
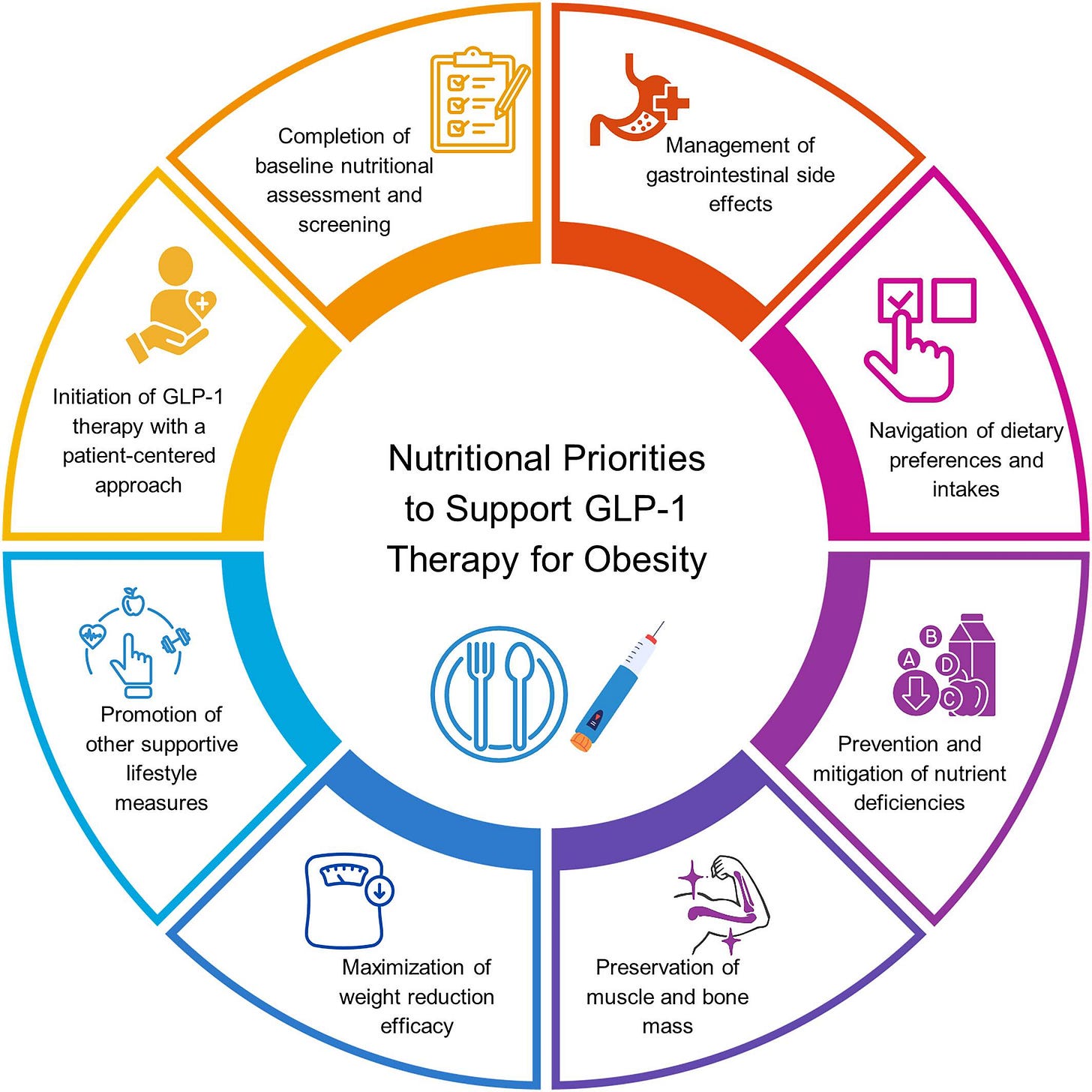
As more patients turn to GLP-1 medications to manage obesity, structured nutrition and lifestyle support has never been more important. A new joint advisory from the American College of Lifestyle Medicine, the American Society for Nutrition, the Obesity Medicine Association, and The Obesity Society offers clear priorities to help clinicians optimise outcomes and mitigate risks.
Here’s a practical summary of key points to apply in practice:
Initiation of GLP-1 therapy with a patient centred approach
Start with a thorough, patient-centred discussion. Ensure patients understand that GLP-1s are an adjunct to lifestyle changes, not a standalone solution. Explore their goals beyond weight alone (e.g. improved energy, mobility, health markers), and screen for barriers such as food insecurity or mental health concerns. Screening for eating disorders is important, noting that restrictive eating disorders are generally a contraindication for GLP-1 use.
Completion of baseline nutritional assessment and screening
A full medical and nutritional assessment should precede initiation. Key checks include: current dietary habits, nutritional status, risk of deficiencies, sarcopenia/osteopenia risk, GI conditions, and psychosocial factors that affect eating behaviour. This is also a time to address any existing nutrient insufficiencies and set realistic expectations for how their appetite and food preferences may change.
Management of gastrointestinal side effects
GI symptoms are common, especially during dose escalation. Proactively counsel patients on smaller, more frequent meals, adequate hydration, and temporary adjustments to food choices to ease nausea and bloating. For constipation, consider increasing fluids and fibre gradually, and using magnesium or other supplements if needed. Help patients avoid the cycle of skipping meals due to nausea, which can worsen symptoms and nutrient intake.
Navigation of dietary preferences and intakes
Expect appetite and food preferences to shift, often away from high fat, high sugar, and ultra processed foods. This can support healthier eating patterns, but reduced interest in food can also risk inadequate nutrition. Encourage nutrient-dense choices and regular eating patterns, and monitor for food aversions or disinterest that could compromise intake. Patients may need support to adjust to their changing relationship with food.
Prevention and mitigation of nutrient deficiencies
Rapid calorie reduction increases the risk of micronutrient deficiencies. Prioritise a diverse diet rich in whole plant foods, lean protein, and healthy fats. Recommend supplementation (e.g. vitamin D, calcium, B12, iron, and multivitamins) as needed, based on individual risk. If appetite is low, small nutrient-dense meals, smoothies, and fortified products can help. Monitor nutrient status regularly.
Preservation of muscle and bone mass
Lean mass loss is a known risk with GLP-1-induced weight loss. To prevent this, protein intake should be optimised with recommendations ranging from 1.2-1.6 g/kg/day during active weight reduction. Some experts suggest 1.5 g per kilogram of lean body mass daily for greater precision. Alternatively, an absolute target of 80-120 grams per day (or 16-24% of total calories on a 2000 calorie diet) may be easier to follow while ensuring adequate intake.
Prioritise high quality protein sources and counsel patients to consume protein first at meals. Equally important is resistance training, at least 3 sessions per week should be encouraged, ideally alongside at least 150 minutes per week of moderate aerobic activity, to preserve muscle and bone health.
Maximisation of weight reduction efficacy
Structured nutrition and lifestyle programs enhance the weight loss effects of GLP-1s. Trials show that intensive lifestyle interventions alongside GLP-1s achieve the greatest weight reductions. Encourage a dietary pattern focused on minimally processed, nutrient dense foods, regular exercise, and behaviour change support (self-monitoring, stress management, sleep optimisation).
Promotion of other supportive lifestyle measures
Don’t forget broader lifestyle factors
Sleep: Poor sleep undermines GLP-1 efficacy, assess and address where needed.
Stress management: Chronic stress can drive weight regain; consider CBT or mindfulness based interventions.
Substance use: Screen for and address alcohol or other substance use that may interact with GLP-1 therapy.
Social support: Foster social connection through group visits, peer support, or structured programs, as isolation is a risk factor for poor outcomes.
The opportunity for dietitians
With structured nutritional care still underutilised alongside GLP-1s, this is a key opportunity for dietitians to lead. Nutrition counselling can enhance efficacy, prevent side effects, preserve lean mass, and support long term maintenance after medication is tapered or stopped. GLP-1 therapy without this support risks weight regain, nutrient issues, and poor patient experience.
Read the full paper 👇
https://onlinelibrary.wiley.com/doi/10.1002/oby.24336
Reference
Mozaffarian D, Agarwal M, Aggarwal M, Alexander L, Apovian CM, Bindlish S, Bonnet J, Butsch WS, Christensen S, Gianos E, Gulati M, Gupta A, Horn D, Kane RM, Saluja J, Sannidhi D, Stanford FC, Callahan EA. Nutritional priorities to support GLP-1 therapy for obesity: A joint Advisory from the American College of Lifestyle Medicine, the American Society for Nutrition, the Obesity Medicine Association, and The Obesity Society. Obesity (Silver Spring). 2025 May 30. doi: 10.1002/oby.24336. Epub ahead of print. PMID: 40445127.
Thanks for reading!
Leif
Got feedback? Email leif@glp1dietitianhub.com, I'd love to hear from you.
Note: This newsletter is for educational purposes only and should not be considered medical advice. Always consult a qualified healthcare professional for personalised guidance.
Subscribe for free to receive new posts and support my work